Introduction
As we approach the end of this year, facing yet another wave of COVID-19, I want to thank you first for your great patient care, and second for your participation in C3. It has not been an easy task to continue the work of value-based care in the midst of shifting health care landscape. But keeping patients healthy, and out of the hospital, is what we signed up for when we chose to be primary care providers. And value-based care is how we get paid for that work.
C3 practices have accomplished much this year, including:
- Helping more than 12,000 women get their mammogram.
- Screening more than 13,000 patients for colon cancer.
- Getting more than 4,000 diabetic patients in for care.
- Conducting more than 18,000 annual wellness visits.
- Checking in with more than 14,000 patients about their emotional state.
Additionally, on the financial side of the house, our practices achieved shared savings in all of our 2020 contracts, resulting in a total payout of more than $15 million to network practices this fall for the work done in 2020.
As we start to come out of the pandemic, it is increasingly evident that value-based payments help to create more sustainable primary care, which results in healthier patients. We look forward to supporting you where we can as we do this work together.
In this newsletter, you will see the progress that has been made this year, as well as new tips about how to continue this work. We hope you find this information useful, and we welcome your feedback as we go into the new year.
Thank you again for all you do!
Amy
Welcome new members
Please join us in welcoming our newest members! Established in 1974, The Family Clinic of Fort Collins is a 5 doctor and 1 NP practice in Fort Collins. They have deep community roots and experience in doing the work of value-based care. We are very excited to have them as part of the network!
Single scorecard and metrics
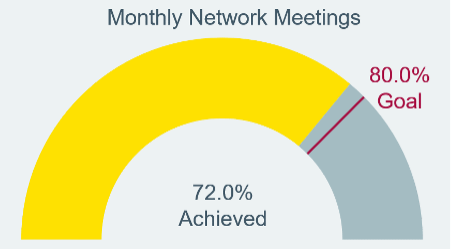
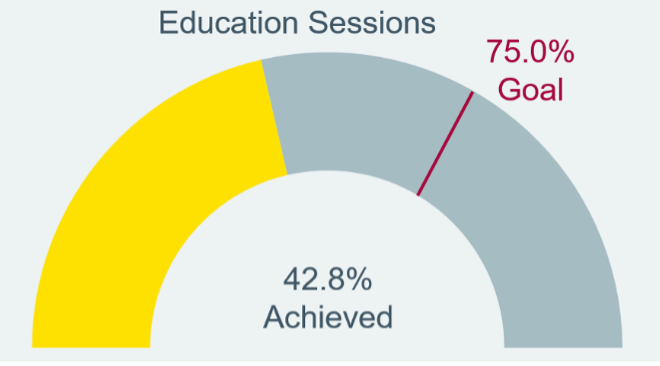
Commitment: We continue to meet with our practices monthly, and are seeing great engagement with the teams on the ground. Additionally, 16 out of our 23 practices have already reached the 75% Educational Sessions goal! We appreciate these efforts and hope you all find the learnings valuable.
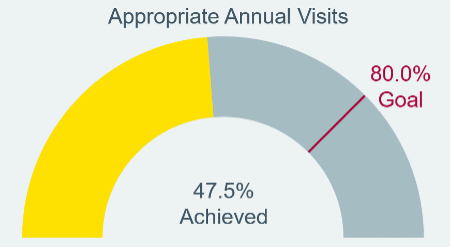
Capabilities: Despite the offices being busier than ever as patients come back to see their doctor for acute and chronic issues, our practices continue to work on getting patients in for their annual visits. We continue to encourage these visits as a way to address the preventative issues that sometimes get missed in the noise of more pressing care needs.
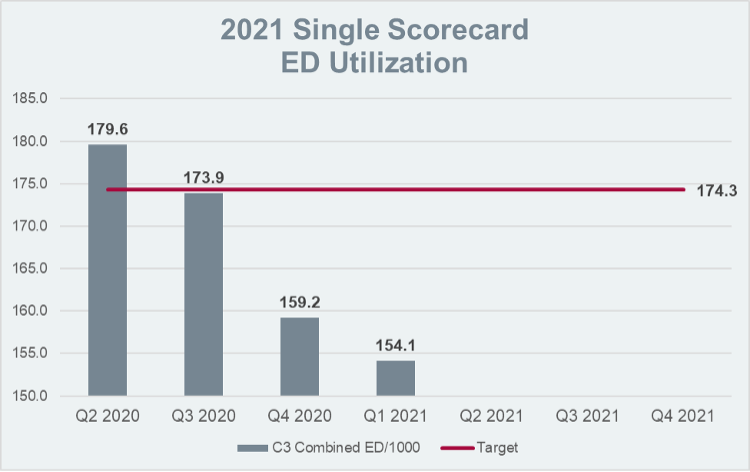
Cost: Finally, we continue to see the pandemic’s effects on our cost and utilization metrics, as patients avoided the ER during the height of the pandemic. We expect these numbers to bounce back (and our practices are telling us they are), and we continue to work hard with our care coordination teams to help patients make choices about where to go for care. Our pharmacy teams are also working with the practices to help identify places where a switch to a generic medication might be appropriate.
Education
Thank you everyone for your ongoing engagement in our Educational Sessions during this year. We know that it was another demand on your time during a year when even more was asked of you. We have taken that into account, and made some exciting changes for 2022 as a result of your feedback.
Education around how to succeed in value-based care remains an important focus of the single scorecard, and we have expanded the scope of this measure to include interactive town halls. Town halls will be conducted quarterly in a virtual forum, focus on topics that have important relevance to success in value-based care, and offer an opportunity for an interactive Q&A session. Additionally, we will continue to add recorded videos in lecture format to the education library. All events will qualify for CME credit.
If you have not yet completed your 2021 education requirement, please visit our website to access recorded videos. CME credit can be requested through our third-party vendor, Eeds. If you need instruction on how to do this, you may access the tip sheet here.
Care management
Care managers support decreasing cost.
Care managers are part of the value-based health care team. They work in the “in-between spaces” with patients and their providers to identify patients who use the emergency room frequently, and address the root cause for ED overutilization. They provide tools for better managing care needed in the home and educate patients about seeking care at the right time and place. This has become even more important during the pandemic, as patients are discharged from hospitals and sent home from the ED with higher acuity levels than they were pre-pandemic. Care managers identify and reach out to those patients who are high risk for readmission and provide them with extra support.
Patients with COVID-19 and anxiety.
Following a diagnosis of COVID-19, and especially a hospitalization for COVID-19, we are seeing high rates of patients with anxiety due to symptoms, stigma and social isolation. The following story highlights how important a care manager can be in addressing this and helping patients feel more confident they are still being cared for, even if they are outside the ED.
ED visit:
Patient was diagnosed with COVID-19 in the ED. Following his visit, he was experiencing shortness of breath, fever and anxiety related to the acute symptoms and diagnosis. He returned to the ED later that same day with the same symptoms.
Care manager call:
Following his ED visits, the patient was contacted by the C3 RN care manager. The patient described having severe anxiety related to his symptoms and diagnosis. He had recognized the need for help and found an outpatient behavior health program and was waiting to be connected with a provider for counseling.
RN care manager intervention:
The RN care manager informed the primary care clinic of patient’s ED visits, diagnosis and his plan to connect with a behavioral health counselor. The care manager also arranged a follow-up visit for the patient with his primary care provider. The care manager supplied the provider with the ED notes and a summary of the conversation with the patient. The care manager confirmed the patient’s follow-up with the psychiatrist and contacted the patient weekly to track symptoms and reinforce the plan of care.
The C3 central care management team works with network practices by outreaching patients following hospitalizations and ED visits. If you want to meet your C3 care manager, please contact Jenn Countryman.
Pharmacy
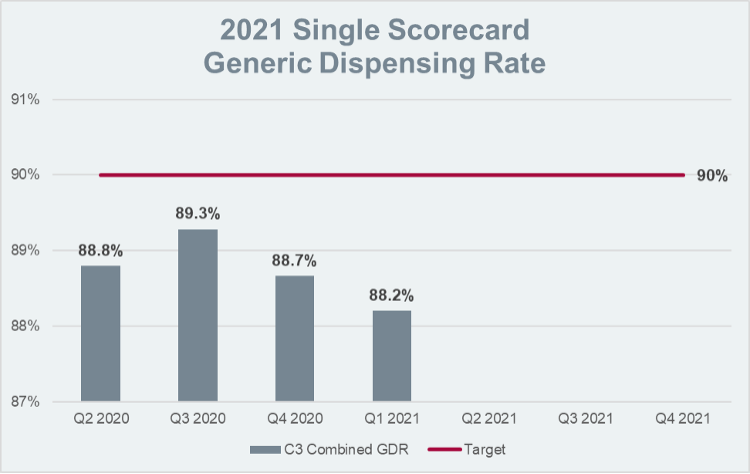
Optimizing medication use is an important aspect of value-based care. The 2021 single scorecard includes generic dispensing rate as a “cost” performance metric and in 2022, medication adherence to statins in patients with diabetes will be added as a “clinical” performance metric.
Generic dispensing rate:
Generic medications not only save the health system valuable health care dollars, they are also often much less expensive for patients. It is estimated that only 39% of branded medication copays are under $20. By comparison, 90% of generic medication copays are under $20.1
The Dirty Dozen list identifies 12 common high-cost, brand-name medications that do not generally provide additional therapeutic benefit over their generic alternatives. This list can be a useful tool to identify common brand-name medications you may be prescribing, as well as recommended alternative medications to consider. Changing a medication on this list to a lower-cost generic has the potential to save anywhere from $1,000 to $60,000 annually, depending on the medication.
Statin adherence in patients with diabetes:
Statins are among the most effective medications in reducing the risk of cardiovascular disease. Using statin therapy in patients with diabetes is estimated to prevent one vascular event for every 15-32 patients treated for 3-5 years.2,3 However, a major barrier to statin benefits is nonadherence. Fifty percent or more of patients have been estimated to be nonadherent to statins after one year.4-6
One practical tip to improve statin adherence is prescribing a 90-day supply and/or using a mail order pharmacy. This increases the amount of medication patients have on hand and limits the number of trips patients need to take to the pharmacy.
Risk Coding
Type 2 Diabetes Mellitus with Complications
When coding for patients with diabetes, it is very important to use codes that account for the whole clinical picture—especially the complications associated with diabetes. Start with E11, the code for diabetes, and use the digits following the decimal point to increase your specificity:
| Fourth Digit | Body Region | Example of ICD 10 |
Description | RAF | Additional Information |
| 2 | Kidney complications | E11.22 | Type 2 diabetes with chronic kidney disease | 0.302 | Still need to code the kidney stage, e.g., N18.31 |
| 3 | Vision complications | E11.311 | Type 2 diabetes with diabetic retinopathy and macular edema | 0.302 | |
| 4 | Neurological complications | E11.42 | Type 2 diabetes with polyneuropathy | 0.302 | |
| 5 | Circulatory complications | E11.51 | Type 2 diabetes with peripheral vascular complications | 0.302 | |
| 6 | Other specified complications | E11.65 | Type 2 diabetes with hyperglycemia | 0.302 | Recommended to use when your patient has “uncontrolled” Type 2 diabetes. |
| 9 | Unspecified | E11.9 | Type 2 diabetes, with no complication | 0.105 |
Contracting
As we demonstrate growing strength in our value-based care efforts as a network, our contracting team has been working hard to ensure that our contracts for 2022 offer greater opportunities for financial success. The payer agreements we are participating in for calendar year 2022 are outlined here. If deemed eligible by the payer, your practice will be required to participate in all of the 2022 C3 commercial agreements. In 2024, the same will be true for the C3 Medicare Advantage agreements. Our network is now managing close to 200,000 lives in these value-based agreements, and we are grateful for your hard work in contributing to the network’s success!
Revenue Opportunities
| Payer | Prospective Per Patient Care Coordination Fees | Annual Shared Savings/ Quality Incentives |
| Aetna Medicare Advantage | X | |
| Anthem Commercial Cooperative Care | X | X |
| Anthem Medicare Advantage | X | X |
| Cigna Commercial Collaborative Accountable Care (CAC) | X | X |
| Cigna Medicare Advantage Partnership for Quality Program (P4Q) | X | X |
| United Commercial | X | X |
| United Medicare Advantage | X |
It is important to note that our Anthem Commercial contract has a component of downside risk starting in 2022. This means that we, along with our payer partner, are accountable should the cost of care for those patients be higher than the funds received to cover that care. As you may be aware, C3 has been preparing for this by creating a reserve pool of dollars to be used if we need to pay money back to Anthem, so that individual practices will not be affected. And, at the practice level, your focus on annual wellness visits, keeping patients healthy and out of the emergency room, and using generic medications when appropriate will help us continue our positive performance.
Finally, as we look to the future and broadening our value-based opportunities, we are exploring other payer offerings as well as value-based Medicare offerings. You will hear more about this throughout 2022.
- Association for Accessible Medicines. accessiblemeds.org/resources/blog/2017-generic-drug-access-and-savings-us-report
- CARDS Trial. Lancet. 2004; 364 (9435): 685.
- HPS Substudy. Lancet. 2003; 361 (9374): 2005.
- Lemstra et al. Proportion and risk indicators of nonadherence to statin therapy: a meta-analysis. Canadian Journal of Cardiology. 2012; 28: 574.
- Mann et al. Predictors of non-adherence to statins: a systematic review and meta-analysis. Ann Pharmacother. Ann Pharmacother. 2010; 44 (9): 1410.
- Benner et al. Long-term persistence in use of statin therapy in elderly patients. JAMA. 2002; 288 (4): 455.