Leadership Message
Colleagues,
In 2020, 34.2 million people in the United States were diagnosed with diabetes—10.5% of the population. Diabetes impacts patients of all social, economic and ethnic backgrounds. It was the seventh leading cause of death in 2017, and the total estimated costs of diagnosed diabetes was $327 billion that year. These numbers have been rising steadily in the past decade, and during the pandemic, it became apparent just how much having diabetes, especially uncontrolled diabetes, impacts patient outcomes in almost every other comorbid condition.
This year, C3 is putting diabetes care at the center of our scorecard. We believe that by focusing on diabetic outcomes, and ensuring these patients are well-supported and taken care of, we can not only improve a broad range of clinical outcomes, but also create savings in our value-based contracts. This quarter’s newsletter offers a range of tips for success as we do this work. We hope you find it valuable for both you and your patients.
Source: Centers for Disease Control National Diabetes Statistics Report 2020; National Institutes of Health
From diabetesresearch.org/diabetes-statistics
Risk Coding
Patients with diabetes are at increased risk of developing peripheral vascular disease (PVD) and/or peripheral arterial disease (PAD). If you determine that your patient has a compromised vascular system, you should appropriately code and document this condition during your patient’s encounter.
If the patient has skin breakdown, or ulcers, from poor circulation or diabetes, you want to make sure to include this diagnosis code and documentation as well.
Did you know that a diabetic patient with peripheral vascular disease (E11.51), atherosclerosis of the native arteries of the right leg with ulceration of toes (I70.235) and skin ulcer of foot including toes (L97.509) would have a RAF score of 1.105?
Telling the whole patient story through your coding and documentation does make a difference.
Type 2 Diabetes Medication: Balancing Cost and Value
Appropriate medication therapy for type 2 diabetes is important for success in value-based care. A1c control, medication adherence and medication costs are metrics that many payers evaluate. However, managing these medications can be challenging, especially when insurance coverage and cost can vary significantly from patient to patient. After optimizing metformin, most patients will require a second-line agent for glycemic control. Dipeptidyl peptidase-4 inhibitors (DPP4i), glucagon-like peptide-1 receptor agonists (GLP-1 RA), and sodium-glucose co-transporter 2 inhibitors (SGLT2i) are commonly used after metformin. These medications are all high cost, so it is important to choose a medication that provides high value if using any of these classes. The table below can assist with selecting patient-specific, high-value medications to optimize value-for-dollar spending for both patients and payers.
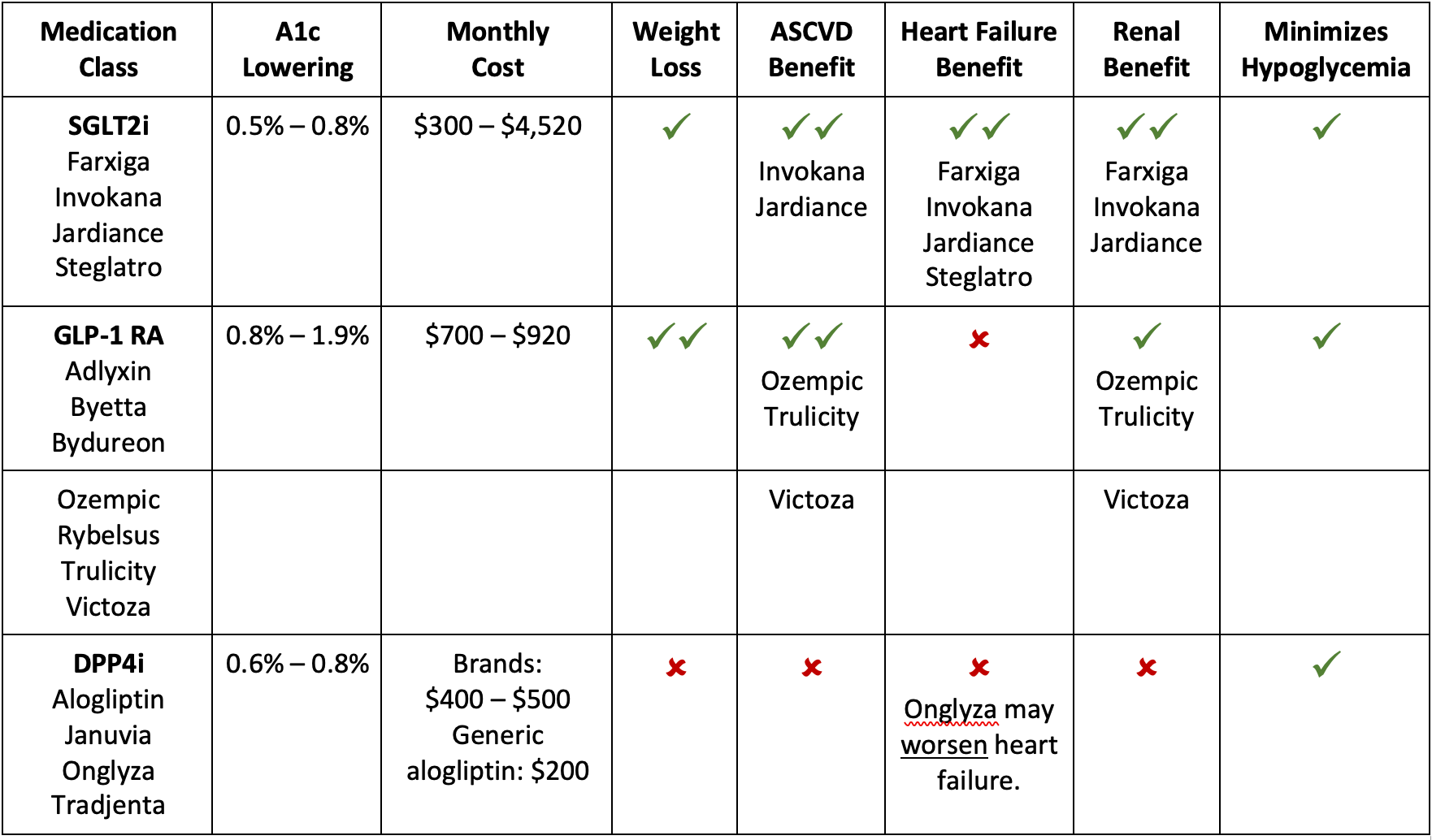
Lower-Cost Options
Some patients have significant affordability concerns that drive the selection of second-line agents and limit the use of DPP4i, GLP-1 RA or SGLT2i medications. The following table provides an overview of the most affordable second-line agents.
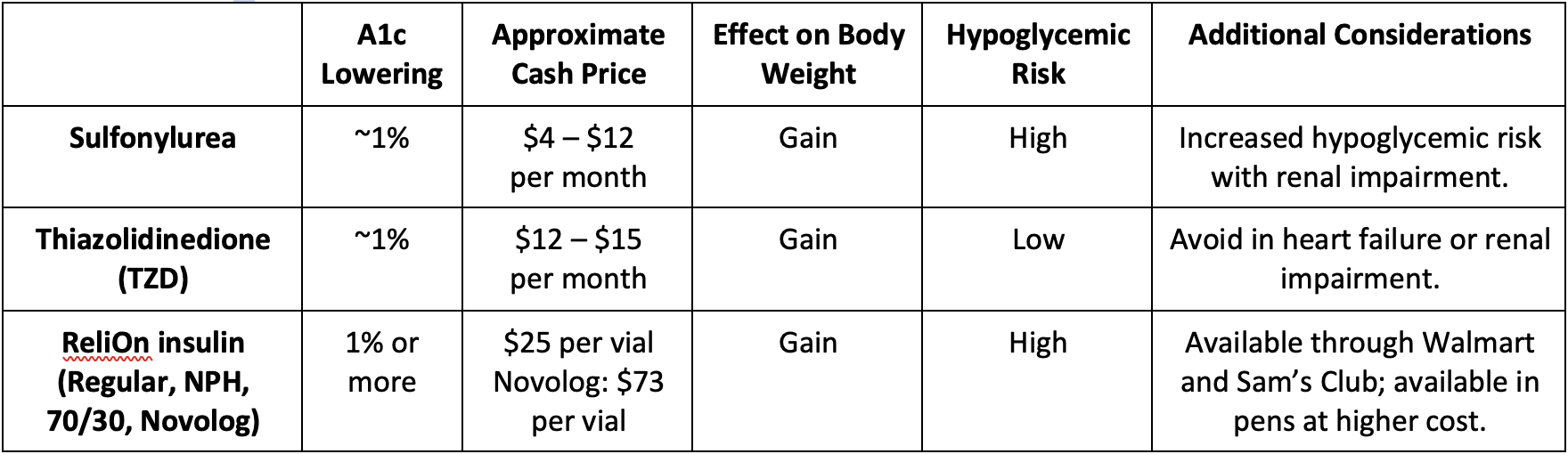
Another option is to consider a combination product. While these often have higher cash prices, for some patients with insurance it results in fewer copays and overall savings compared to single-agent preparations. Patients can contact their insurance company to see if a combination product is more cost-effective for their plan. There are numerous combination products available, and it can be difficult to determine what medication classes are included. The chart below provides an overview of which classes have combination products available.

Additional Resources
The American Diabetes Association 2022 Standards of Medical Care in Diabetes has a section devoted to medication therapy, which provides more detailed information. Consider bookmarking these pages to have a quick reference guide:
Table comparing medication classes on efficacy, weight effects, cardiovascular/renal benefits, cost and dosing information.
Flowchart for selecting medications based on patient-specific needs (cardiovascular/renal concerns, hypoglycemia risk, weight effects, cost).
Flowchart for adding and adjusting injectable therapies, specifically insulin and GLP-1 RA.
References:
American Diabetes Association Professional Practice Committee; 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes—2022. Diabetes Care 1 January 2022; 45 (Supplement_1): S125–S143. https://doi.org/10.2337/dc22-S009
Clinical Resource, Drugs for Type 2 Diabetes. Pharmacist’s Letter/Prescriber’s Letter. December 2020.
Clinical Resource, Comparison of Insulins. Pharmacist’s Letter/Prescriber’s Letter. September 2021. [370901]
Care Managment
Goal setting is a powerful way to help patients create lasting healthy behaviors, especially when they are living with diabetes. Patients are most successful managing their diabetes when they create and define the steps toward the lifestyle changes providers encourage. A care manager can help in this process.
We all know that exercise and diet are two areas that rely on patient behavior and can have a direct impact on diabetes control. While providers can encourage patients during office visits, care managers can follow up with patients after their visit to reinforce what they are being told. They can prompt patients to think about what they would like to do that can increase success. They can provide ongoing support as patients learn to think differently about meals. Care managers can also help patients identify small steps toward change, which can have a huge impact on outcomes.
RN care managers can also help connect patients to education programs, nutrition counseling and support groups, and make sure patients have the appropriate tools and knowledge needed to manage their diabetes. Community centers offer a variety of group classes and involving a spouse or friend in activities can be a good motivator. Cookbooks or nutrition blogs are good resources to find diabetic-friendly recipes. The American Diabetes Association has a library of patient-friendly information, including a podcast. Lastly, there are free and low-cost mobile apps directed at education, nutrition and exercise.
Resource ideas for patients, regardless of which region they live in:
- America Diabetes Association
- YMCA
- American Diabetes Association podcast “Ask the Experts: It’s personal”
- Available on Spotify and iTunes
- Mobile app examples:
- Diabetes Type 2 by Nourishly (free app)
- Diabetes Tracker by MyNetDiary (monthly fee)
- Fooducate (monthly fee)
- My Diabetes Diet & Meal Plan (monthly fee)
If you would like more information about how care managers can support patients with diabetes, please contact Jenn Countryman.
Patient Outcomes
One of the main drivers to succeeding in value-based care is improving quality outcomes for patients. Through the single scorecard and monthly practice meetings, we focus providers and office staff on high-impact and high-value areas across payer contracts.
Many high-impact, high-value areas center around diabetes care, which is why the network heavily focuses on these metrics. We know that these quality metrics can be challenging to address and close throughout the year. To receive tip sheets that walk you through the need-to-know information, please complete and submit the form below.
Payer Feedback
Diabetes care quality measures play a significant role in all of our payer contracts, which is why four of the six metrics on our 2022 Single Scorecard involve the care of patients with diabetes. Success in these metrics will not only lead to better outcomes for our diabetic patients; it will also generate financial success in our value-based contracts.
So, how are we doing according to the payers? The Medicare Advantage data probably tells the story best: We have some work to do, most significantly in the area of diabetes, blood sugar controlled (A1c <8).
Diabetes Care Quality Measures
Medicare Advantage Programs: Star Ratings
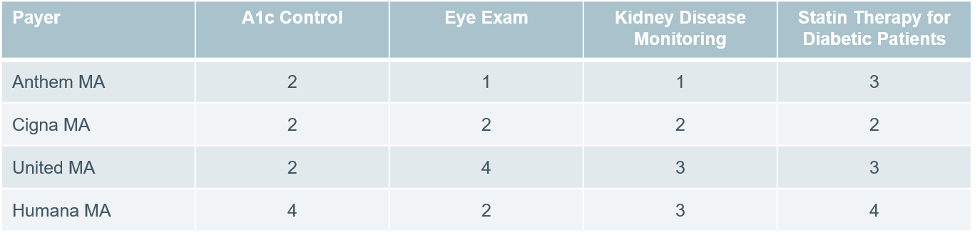
Across our Medicare Advantage programs, C3 performance is only at a 2-star rating for diabetes control. This is below the threshold needed to earn incentives in this metric. Since this is a triple-weighted measure in the MA space, this performance is heavily impacting our overall star ratings so we will continue to focus on this measure throughout the year.
Notes:
- Anthem MA and Humana MA reporting through October 2021; Cigna MA and United MA reporting through November 2021.
- Despite having 4 stars in A1c Control in Humana MA, we are not meeting the minimum target for the model practice quality incentive program.
- Payer-specific measures may not always be identical to Single Scorecard measures.font